MDMA for PTSD & CPTSD
MDMA for Post Traumatic Stress Disorder (PTSD)
& Complex Post Traumatic Stress Disorder (CPTSD)
Did you know that the FDA has completed three trials of a drug that could help those of us with PTSD and CPTSD?
Not an antidepressant taken daily, but a drug you take once with assisted therapy. For over 70% of the participants so far, one treatment took their PTSD away. Cured it. 18 weeks later, over 70% of the people no longer qualified for a PTSD diagnosis.[1]
Like many Americans struggling with depression, anxiety, and post-traumatic stress, I was on Lexapro for over 18 years, starting after my son’s death in 2006. Did it help? It certainly seemed to keep my scary feelings at bay slightly, but after 18 years, I wasn’t achieving any lasting healing, despite the many therapists I continued to talk to. When I received a formal CPTSD diagnosis (2021), I was told my complex trauma was so severe, I’d unlikely ever recover. I think that’s an awful thing to tell someone, and thankfully, I don’t like being told what to do, so it motivated me to keep looking for an answer.
I didn’t just want to heal: I needed to. Most days, I was barely able to get two things done before my body gave out on me. My immune system was so compromised, I would get sick very easily, and recovery was slow. My hair was falling out, my spine hurt almost constantly. I was sober, but very depressed, and I didn’t see a future where I felt physically better. I was hardly 50 years old and I already felt like this? I felt like I had to try harder at least, and since I had good business experience, I decided to treat my CPTSD like a business challenge I wanted to solve. Would I work hard for myself? Was there really nothing more out there that could help me?
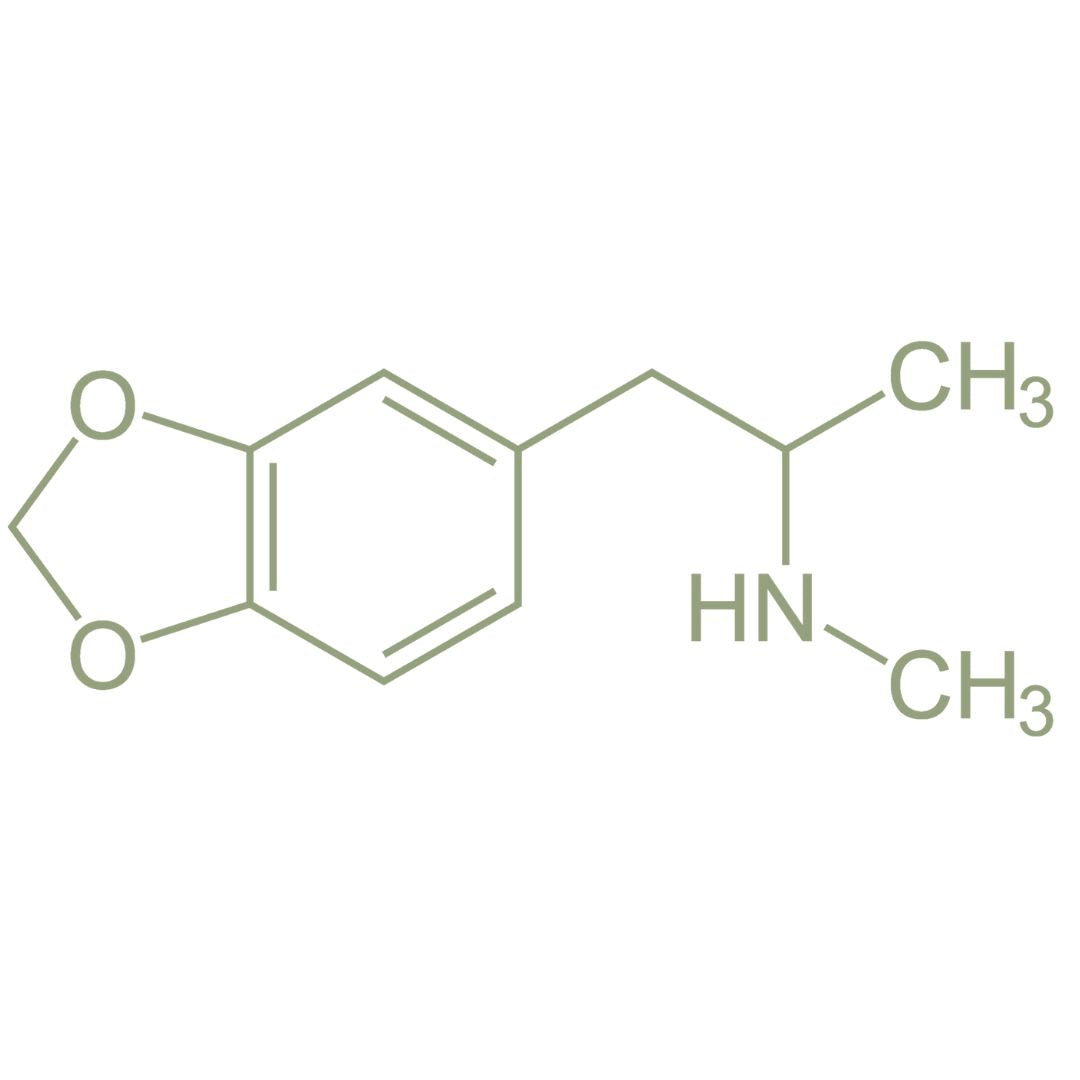
I decided to start with three things: a Ketamine program via Mindbloom, Eye Movement Desensitization Reprocessing therapy, and attendance at PsyCon, a trade show for Psychedelic Research. While at PsyCon, I learned about 3,4-methylenedioxymethamphetamine (MDMA) for PTSD. I was floored at how many people were talking about it.
What I thought I knew as the street drug called ‘Molly’ might have healing properties and could help with my CPTSD? I was shocked and actually burst into tears when I heard the results: 18 weeks post one dose, over 70% no longer qualified for PTSD. [2] After being told there was nothing that could be done for me, I was excited and relieved.
Why is this drug working? MDMA lowers the fear in your brain’s amygdala, allowing scary memories to be reprocessed more easily. The amygdala is an almond-shaped mass of gray matter inside your cerebral hemisphere of your brain. Part of the limbic system, it’s responsible for emotions, survival instincts, and memory. The amygdala helps you process emotions, especially fear and anxiety, by identifying threats and initiating physiological responses, such as fight or flight. If you have trauma, the amygdala can release stress hormones, altering the neurochemistry of your brain, or even disrupting connections between the amygdala and the other brain regions.
What does that feel like? When the amygdala is dysregulated or damaged, life can feel scary even when the trauma is gone. PTSD and CPTSD survivors continue to be haunted by threats from the past, even years later. MDMA temporarily alters your consciousness, reduces fear and increasing emotional connection, thereby promoting a sense of safety. This allows you to face traumatic memories and reconsolidate them through processing. MDMA creates an ideal environment to heal, given the opportunity to lower the fear base and process trauma with support.
Even after learning all that, I wasn’t sure it would work for me: I didn’t feel that scared anymore, and I was willing to talk – I’d talked to everyone I could think of, and approximately twelve therapists later, I was still talking. Would it make a difference? Yet, what followed for me was instrumental to my healing: MDMA allowed me to face things I was hiding from, talk about things I had forgotten, and stop blaming myself for the abuse I suffered.
Since you can’t take MDMA if you are on SSRIs (antidepressants), I had to stop taking Lexapro after 18 years. (SSRIs increase serotonin in your brain. It could be dangerous to overload your system with serotonin, so you need to be clean of SSRIs prior to taking MDMA.) If you’ve experienced antidepressants, you know that they can take weeks to work and have significant side effects: insomnia, diarrhea, sexual dysfunction, headaches, and dizziness. To stop taking an SSRI, it’s recommended that you wean slowly due to the effect on your system. After attending PsyCon and hearing from so many people about how MDMA really works, I didn’t hesitate in my next steps. I weaned myself off Lexapro over a 10-week period preceding my first MDMA session. (Please note, getting off antidepressants is hard and should not be taken lightly. Please use a doctor’s guidance and go SLOW.)
What does an MDMA for PTSD session look like?
An MDMA for PTSD session is guided by a qualified trauma therapist who is literally with you the entire time and a full day is recommended to dedicate to the process. So you are literally spending 6+ hours with someone dedicated to supporting you. A comfy space is recommended and an eye mask, cozy socks and anything to make your body comfortable is prepped before-hand (often called Set & Setting.) For a trauma survivor, this part is amazing and uncomfortable, because while we crave connection it often doesn’t feel safe.
The therapist works with you to set Intentions prior to the “journey” day; a similar post-session meeting helps Integrate what you and your body discovered. During the session, you put on your eye mask and try to “go inside”. Music can be an important part and help soothe you. It’s like a sick day – with allowance to enjoy it and support available.
While my first MDMA for PTSD experience was not phenomenal in understanding what was happening, I immediately noticed a new ease in my thoughts and feelings in the days after. I was able to talk about difficult things, and I understood my own feelings (previously and often, hard to reach). In addition, I found that the lower fear lasted for 8-10 weeks post-session! Trauma lives in the body, not the brain, and my disconnect from my body was so huge I didn’t realize how fearful I remained. I had literally lost touch with my physical body. Post my first MDMA session, I found it so much easier to LIVE. I wasn’t haunted by fearful thoughts or hypervigilant of danger. In my experience, MDMA softens the amygdala’s fear just enough to allow you to see what happened from your adult point of view, not the scary younger point of view you are carrying around. Trauma lives in the body, not the brain, and when we think about it, our bodies think it’s happening again. It’s hard to turn this off and convince your body that you are "safe now”; the body remembers and thinks the trauma is recurring. What results is a constant hyper-vigilant view of the world: always looking for the threat. Walking around on eggshells is not fun and is no way to live every day.
How long have people known this about MDMA? How was it discovered?
- In the late 1970’s Dr. Alexander “Sasha” Shulgin[3], a chemist, synthesized MDMA and reported empathogenic effects: increased feelings of emotional closeness, trust, and reduced fear, which he thought could be useful in therapy. He was right! He worked with Dr. Leo Zeff to start using MDMA in underground therapy sessions. Healing was on the way!
- Yet, in 1985, the DEA classified MDMA as a Schedule 1 drug[4], citing concerns about recreational use. This classification halted most legal research.
- In 1986, Rick Doblin founded the Multidisciplinary Association of Psychedelic Science, or “MAPS” (www.maps.org), for MDMA research. This would begin Rick’s three decades to advocate – fight – for legalization of a drug that could heal so many. [5]
- 2011: MAPS.org completes Phase 1 trials with the FDA; 83% of participants no longer met the criteria for PTSD two months post treatment![6]
- 2017: FDA grants “Breakthrough Therapy” designation for MDMA for PTSD, putting it on an expedited drug development pathway after preliminary evidence supports how MDMA treats a serious and life-threatening condition with a substantial advantage over other treatments. [7]
- 2018: MAPS.org completes Phase 2 trials with FDA oversight: at the 12-month follow up 76% of participants did not meet the PTSD criteria.[8]
- 2021 and 2023: MAPS.org completes Phase 3 trials with the FDA. This time, a double-blind, placebo-controlled, multi-site study was conducted to assess the efficacy and safety of MDMA assisted psychotherapy. 67% of MDMA-treated participants no longer met PTSD criteria at the primary endpoint, vs. 32% in the placebo group.[9] Nature Magazine publishes the results in September 2023.[10]
- 2024: The FDA rejected the approval of MDMA for PTSD – and we just recently, August 2025, received a response on why: despite the FDA selected protocol design of how to conduct the trials, they have shifted their standards regarding “double-blind” studies and demanded more information be gathered.
I agree with Rick Doblin, who says: “the science is clear, the urgency is undeniable and the human suffering is immense”.[11] 13 million Americans live with PTSD; this doesn’t include the millions of us suffering with CPTSD. After almost 40 years advocating for MDMA for PTSD, MAPS.org has administered MDMA to approximately 1700 humans, with one adverse reaction. We need approval for MDMA!
CLINICAL TRIALS:
If you have PTSD or CPTSD, check out the clinical trials to see if there is one near you. You might be able to help pave the way by participating, and a majority (over 70%) of participants no longer qualify for PTSD 18 weeks post one treatment.
If you are a Veteran and suffer from PTSD/CPTSD, check out the VA-funded trials here. VA researchers affiliated with Brown University and Yale University are preparing to evaluate the potential of MDMA for PTSD. [12]
NOTE: If you have a history of a serious psychotic disorder (schizophrenia, borderline personality), please use caution. It’s recommended that you abstain from any hallucinogens.
[1] Phase 1 results 83% of participants no longer had a PTSD diagnosis; Phase 2 over 76% and Phase 3 over 67%
[2] Phase 1 results 83% of participants no longer had a PTSD diagnosis; Phase 2 over 76% and Phase 3 over 67%
[3] https://shulginresearch.net/about/sasha_shulgin/
[4] https://www.nytimes.com/1985/06/01/us/us-will-ban-ecstasy-a-hallucinogenic-drug.html
[5] https://maps.org/about-maps/#history
[6] https://maps.org/news/bulletin/maps-research-update-summer-2011/?utm_source=chatgpt.com
[7] https://pmc.ncbi.nlm.nih.gov/articles/PMC6751381/
[8] https://pubmed.ncbi.nlm.nih.gov/30371148/
[9] https://maps.org/2017/08/22/phase-3-program/?utm_source=chatgpt.com
[10] https://www.nature.com/articles/s41591-023-02565-4
[11] https://maps.org/2025/09/04/fda-public-release-of-crl/
